Evidence-based Clinical Guidelines for Opioid Use Disorder
Published Materials
- Summary Brochure – Introduction to OUD
- Summary Brochure – Prescribing buprenorphine
- Evidence Document
- Reference Card – OUD basics
- Reference Card – Prescribing buprenorphine
- Patient Brochure
- Tear Off – OUD basics
- Tear Off – Starting buprenorphine at home
- Poster
Nearly 3 million Americans have opioid use disorder (OUD), but only 1 in 10 receive treatment.1,2
This module helps primary care clinicians identify and diagnose patients with opioid use disorder, understand the role of medication for OUD, learn a process to initiate buprenorphine in patients with OUD, and learn about harm reduction strategies, including recommending or prescribing naloxone.
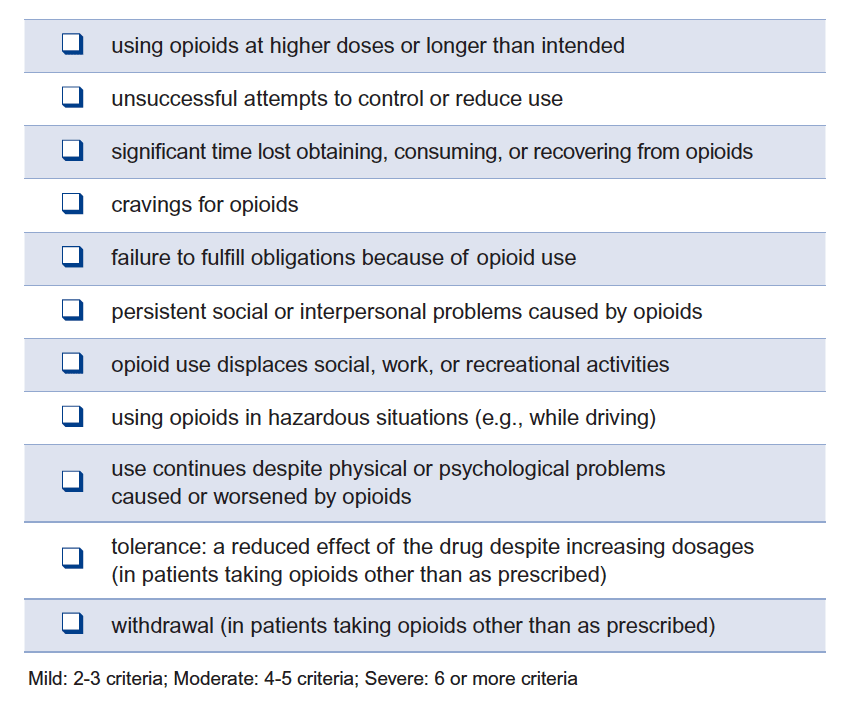
Defining opioid use disorder
OUD is problematic opioid use that leads to clinically significant impairment or distress. It is marked by at least two of the following over the past 12 months.3
OUD results from a combination of factors such as environment, biology or genetics, and the drug used.4 Treatment can be managed with effective medications.
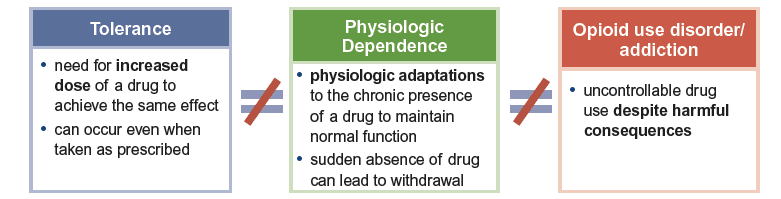
Opioid dependence does not equal opioid addiction5
Patients who take opioids as prescribed without impairment of daily life do NOT have an addiction.
Primary care providers play an integral role in identifying patients with OUD. Adding questions about opioid misuse to annual screening questions about tobacco and alcohol create an opportunity to discuss or uncover problematic behaviors. Screening, Brief Intervention, and Referral to Treatment (SBIRT) provides a framework for assessing patients reporting problematic behaviors, engaging patients in behavior change, and linking them into any needed treatment.5
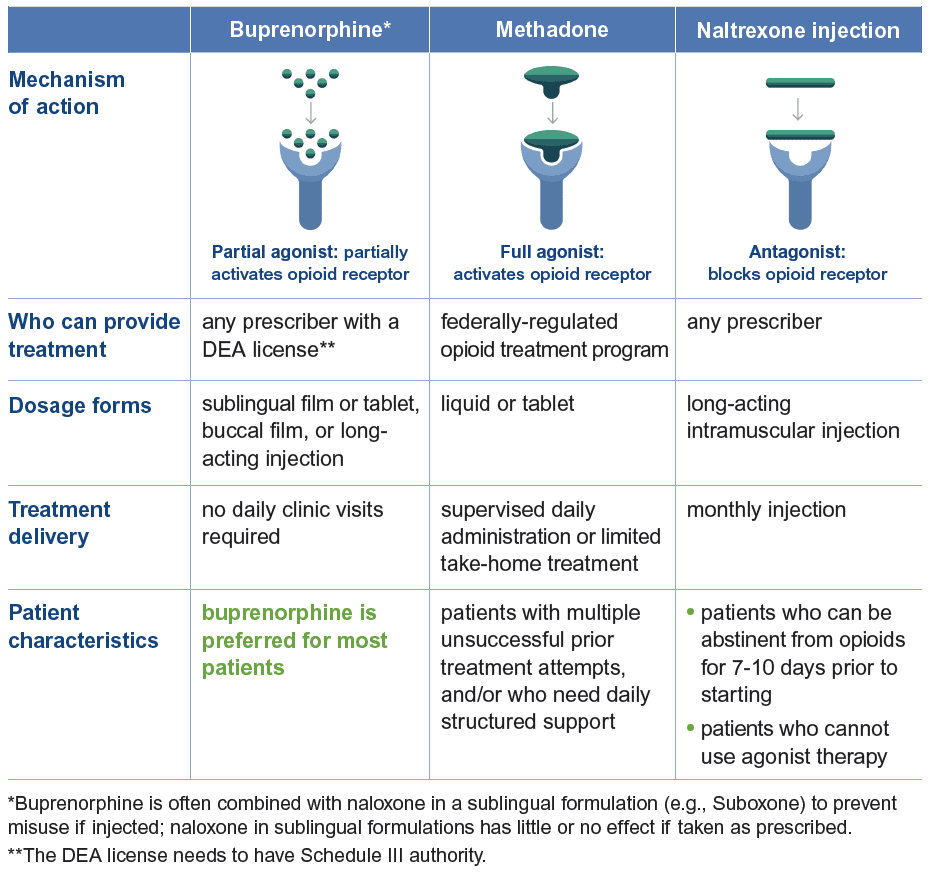
Medications to treat OUD
Three medications are FDA-approved to treat OUD: buprenorphine, methadone, and naltrexone extended-release injection. All of these options can improve retention in treatment, increase time without opioid misuse, and reduce mortality.
Tailor the choice of medication to the patient
Buprenorphine is one of the most effective interventions available. For every 5 people treated with buprenorphine for OUD, 1 life will be saved.6 Buprenorphine can safely be initiated at home in many patients. See the Buprenorphine Initiation sheet above for step-by-step instructions on starting treatment at home.
Clinicians can treat OUD with medication even without access to concurrent behavioral treatment.7,8
Harm reduction
Implement strategies to reduce the risk of overdose or morbidity from OUD.
- Prescribe or discuss naloxone.
- Recommend routine immunization, especially for hepatitis, pneumococcus, and tetanus.
- Screen for infections, especially HIV and hepatitis C.
- For patients who typically use alone, recommend www.neverusealone.com or the 1-800-484-3731 hotline to prevent unintentional overdose.
- Discuss sterile injection practices to reduce transmission of blood-borne pathogens like HIV and hepatitis C, link with a syringe exchange program (if available), or prescribe insulin needles.
- Recommend fentanyl test strips, if available.
- Evaluate whether pre-exposure prophylaxis (PrEP) is indicated for HIV prevention.
Resources for Providers
- Prescribing Naloxone
- What is SBIRT?
- SBIRT Billing
- Tobacco, Alcohol, Prescription medication, and other Substance use (TAPS) Tool
- Drug Abuse Screening Tool (DAST-10)
- Providers’ Clinical Support System
- Find a buprenorphine prescriber
- Clinical opiate withdrawal scale (COWS)
Buprenorphine Updates
State specific resources
- Georgia – Intervention and treatment resources
- Illinois – Intervention and treatment
- Illinois – Find treatment assistance at 1-833-2FINDHELP
- Kansas – Treatment resources
- Missouri – Medication assisted treatment resources
- Missouri – NoMOdeaths Harm reduction resources
- Ohio – Treatment resources
- Oklahoma – Treatment services
- Oklahoma – OK I’m Ready treatment resources
- Pennsylvania – Treating heroin and opioid addiction
- Pennsylvania – Opioid dashboard
- Texas – Opioid treatment resources
- Virginia – Opioid dashboard
Information current at time of publication, February 2023.
The content of this website is educational in nature and includes general recommendations only; specific clinical decisions should only be made by a treating clinician based on the individual patient’s clinical condition.
References
- NIDA. Overview. National Institute on Drug Abuse website. https://nida.nih.gov/publications/research-reports/medications-to-treat-opioid-addiction/overview. January 21, 2022. Accessed April 6, 2022.
- Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: Results from the 2020 National Survey on Drug Use and Health. Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration;2021. HHS Publication No. PEP21-07-01-003, NSDUH Series H-56.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th Ed., Text Revision. Arlington, VA: American Psychiatric Publishing; 2022.
- National Institute on Drug Abuse. Drug misuse and addiction. https://nida.nih.gov/publications/drugs-brains-behavior-science-addiction/drug-misuse-addiction. Published July 13, 2020. Accessed February 23, 2022.
- Szalavitz M, Rigg KK, Wakeman SE. Drug dependence is not addiction-and it matters. Ann Med. 2021;53(1):1989-1992.
- Larochelle MR, Bernson D, Land T, et al. Medication for Opioid Use Disorder After Nonfatal Opioid Overdose and Association With Mortality: A Cohort Study. Ann Intern Med. 2018;169(3):137-145.
- National Academies of Sciences E, Medicine;. Medications for Opioid Use Disorder Save Lives. Washington, DC: The National Academies Press; 2019.
- Fiellin DA, Barry DT, Sullivan LE, et al. A randomized trial of cognitive behavioral therapy in primary care-based buprenorphine. Am J Med. 2013;126(1):74.e11-77.