CME credit available from Harvard Medical School through 2025.
Published Materials
- Summary Brochure
- Evidence Document
- Reference Card
- Tear Off
- Brochure – Fall Prevention – Check For Safety
- Brochure – Fall Prevention – CheckForSafety (Spanish)
- Brochure – Fall Prevention – What You Can Do
- Brochure – Fall Prevention – What You Can Do (Spanish)
This module helps primary care clinicians identify and manage patients with osteoporosis, understand the role of medication to prevent fracture, and utilize non-pharmacologic interventions such as calcium and vitamin D, fall prevention, exercise, smoking cessation and limiting alcohol consumption.
Low bone mineral density is common. Over 10 million Americans age 50 and over have osteoporosis, with as many as 43 million more with osteopenia.1 Decreased bone mineral density puts patients at risk of debilitating falls and fractures.
Dual-energy x-ray absorptiometry (DXA) is a quick and easy way to identify patients with reduced bone mineral density.
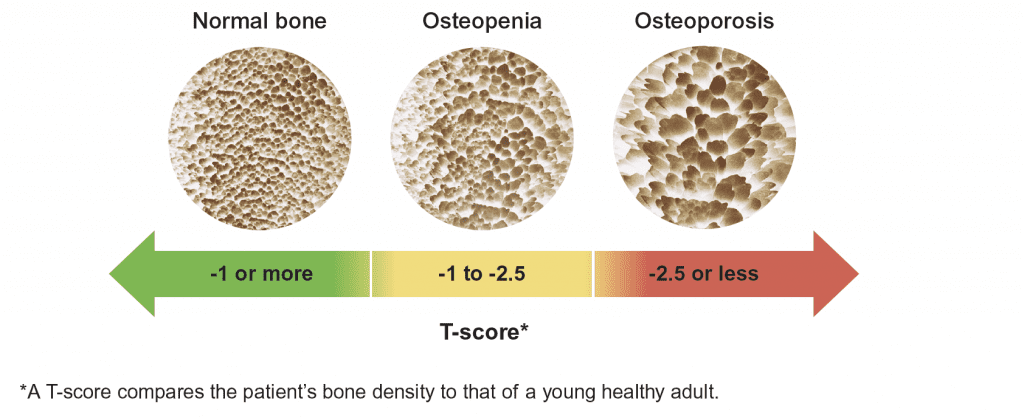
Use the T-score to identify patients with osteopenia or osteoporosis.2,3
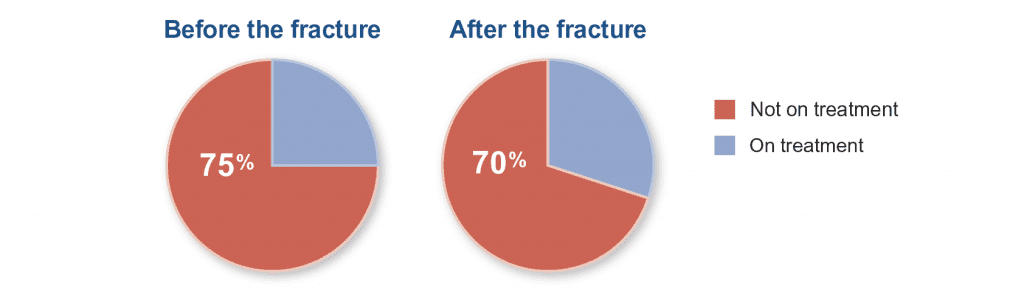
A history of an osteoporotic fracture (e.g., a break to a bone from a fall of no more than standing height) can also indicate osteoporosis. Around 1.5 million Americans have an osteoporotic fracture each year.4 Despite this, many patients are not started on treatment after the fracture to reduce the risk of subsequent fracture and stabilize or increase bone mineral density.
Opportunities remain to initiate treatment for osteoporosis5
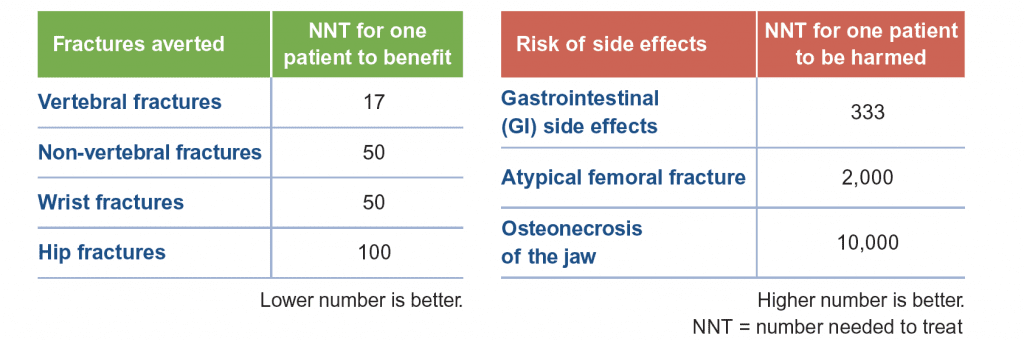
Treatment for osteoporosis for many patients will be a bisphosphonate. This class of medications is effective at reducing fracture.
The benefits of bisphosphonates generally outweigh the risks6-9
While atypical femoral fractures and osteonecrosis of the jaw have been associated with bisphosphonates, these side effects are rare and should not limit treatment.
Treatment selection and duration are driven by patient specific factors. See the Summary Brochure above for more information.
Non-pharmacologic options to improve bone strength
- Ensure adequate calcium intake and vitamin D levels
- Calcium: Patients should take in about 1,200 mg per day of calcium, preferably from the diet
- Vitamin D: Maintain serum vitamin D levels between 30-50 ng/mL, using supplementation – up to 4,000 international units of vitamin D3 per day, if needed
- Prevent falls
- Identify patients with elevated fall risk using the Timed Up and Go (TUG) test
- Review other common reasons for falls, referring patients to additional resources and supports as needed.
- Stay active with a combination of resistance and weight-bearing exercises
- Avoid heavy alcohol use
- Stop smoking
Resources for Providers
Resources for Patients
- Falls prevention in older adults
- Fall prevention program
- Strength and balance program
- Fall prevention guide
- Fall prevention checklist
- CDC STEADI resources
Information current at time of publication, August 2022.
The content of this website is educational in nature and includes general recommendations only; specific clinical decisions should only be made by a treating clinician based on the individual patient’s clinical condition.
References
-
Wright NC, et al. J Bone Miner Res. Nov 2014;29(11):2520-6.
-
Siris ES, et al. Osteoporos Int. May 2014;25(5):1439-43.
-
Rani S, et al. Biosensors (Basel). Apr 21 2020;10(4):42.
-
Clynes MA, et al. Br Med Bull. May 15 2020;133(1):105-117.
-
Yusuf AA, et al. Arch Osteoporos. Dec 2016;11(1):31.
-
Bauer DC, et al. Arch Intern Med. 2000;160(4):517-525.
-
Wells GA, et al. Cochrane Database Syst Rev. Jan 23 2008;(1):Cd001155.
-
Shane E, et al. J Bone Miner Res. Jan 2014;29(1):1-23.
-
Khan AA, et al. J Bone Miner Res. Jan 2015;30(1):3-23.