Pain is one of the most common reasons for visits to primary care providers every year. Yet, despite the prevalence, managing pain remains a significant challenge. Current recommendations for addressing chronic pain focus on a multi-modal approach including non-pharmacologic and pharmacologic treatments. This module discusses the evidence-based management options for four common pain conditions: osteoarthritis, low back pain, diabetic neuropathy, and fibromyalgia. It includes recommendations for managing patients who may require or already be taking opioids including monitoring opioid safety and reducing opioid overdose risk by prescribing naloxone.
Overview for managing patients with non-cancer pain
Managing pain requires establishing clear functional goals that center on activities which are important to each patient. In order to achieve these goals, a focus on non-opioid treatment options is recommended. For those patients who do require opioids, utilizing non-opioid options can reduce total opioid doses and help improve function.
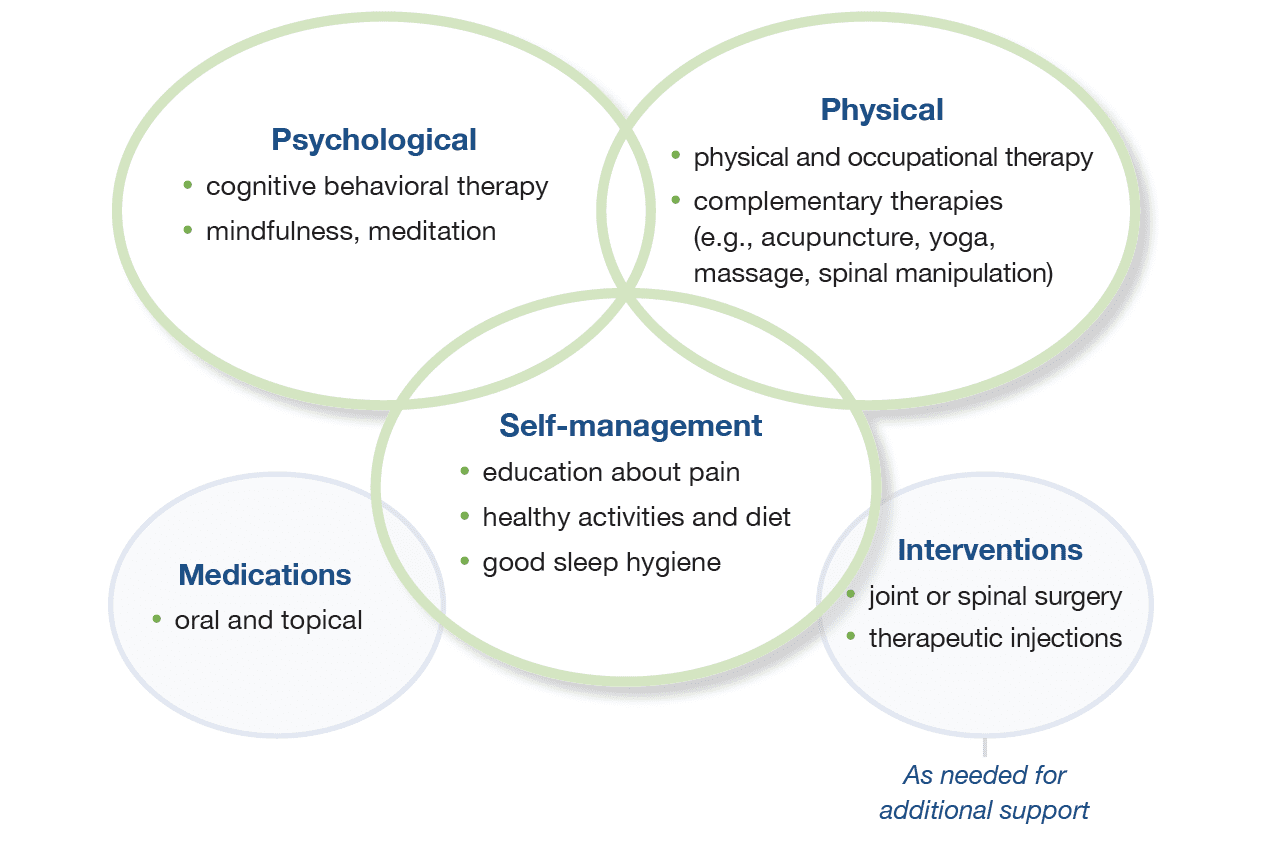
Combine different ways to improve function and alleviate pain1
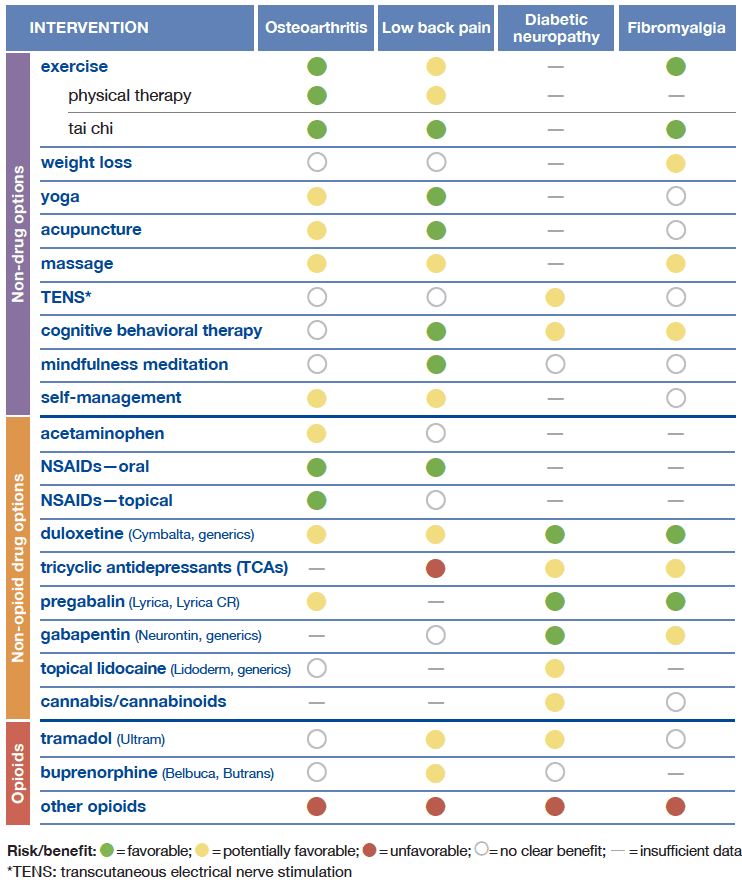
Selecting evidence-based treatment options can be challenging, with some pain conditions having more options available to manage pain than others. Below is a summary of common options used to manage pain and a corresponding benefit to risk profile for each option. For more details regarding the evidence behind these recommendations, please see the comprehensive evidence document.
Evidence-based recommendations for managing specific chronic pain conditions
A note on opioids
Tramadol is an opioid with activity at serotonin and norepinephrine receptors. It can still cause withdrawal symptoms like other opioids and has drug interactions. Buprenorphine is a mixed agonist that has a ceiling effect on respiratory depression with escalating doses. This effect reduces the risk of overdose from buprenorphine alone. Thinking about one of these two options may be a safer opioid option than starting with full agonist options.
Managing patients on opioids
While opioids are not generally recommended for these four pain conditions, many patients already use opioids to manage pain. For these patients and others who may require a trial of an opioid medication, ensuring safety is critical. These steps are recommended for all patients taking opioids:2
- Set clear functional goals with the patient
- Establish an anticipated duration of opioid use
- Establish a written treatment agreement
- Routinely assess the risk and benefits of opioid use
- Continue to optimize non-opioid treatment options
- Prepare to taper off opioids and pursue other modes of analgesia if goals are not met
Reducing opioid doses
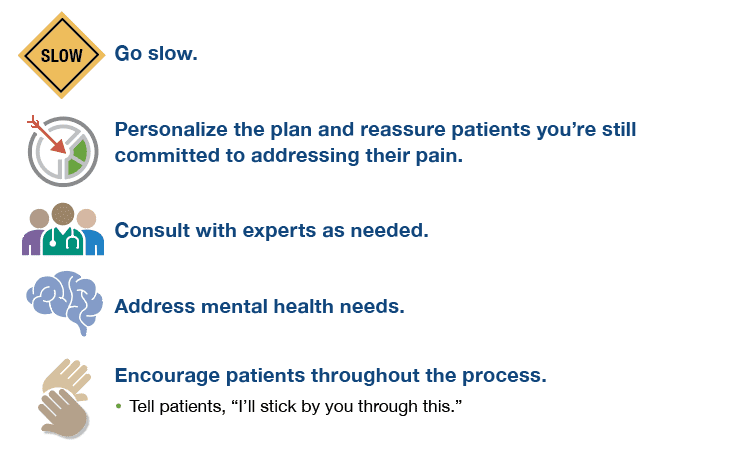
Decisions to taper treatment should be individualized and patient-centered.2,3
Resources for Providers
State specific resources
- Georgia: Opioid response
- Illinois: Prescription opioids and heroin
- Illinois: Medical cannabis
- Missouri: Medical cannabis
- Ohio: Opioid prescribing guidelines
- Ohio: Naloxone – Project Dawn
- Oklahoma: Prescribing guidelines
- Oklahoma: Naloxone resources
- Pennsylvania: Opioid epidemic
- Pennsylvania: Medical marijuana
- Texas: Opioid training initiative
Click here to contact us for more information about Alosa’s full academic detailing package.
